Platform
Our fully-configurable platform automates all of the important aspects of building and maintaining a network of aging-in-place providers. Our software seamlessly handles provider credentialing, referral management, fulfillment tracking, claims processing, and automatic auditing. This enables you to focus on what truly matters: member satisfaction.

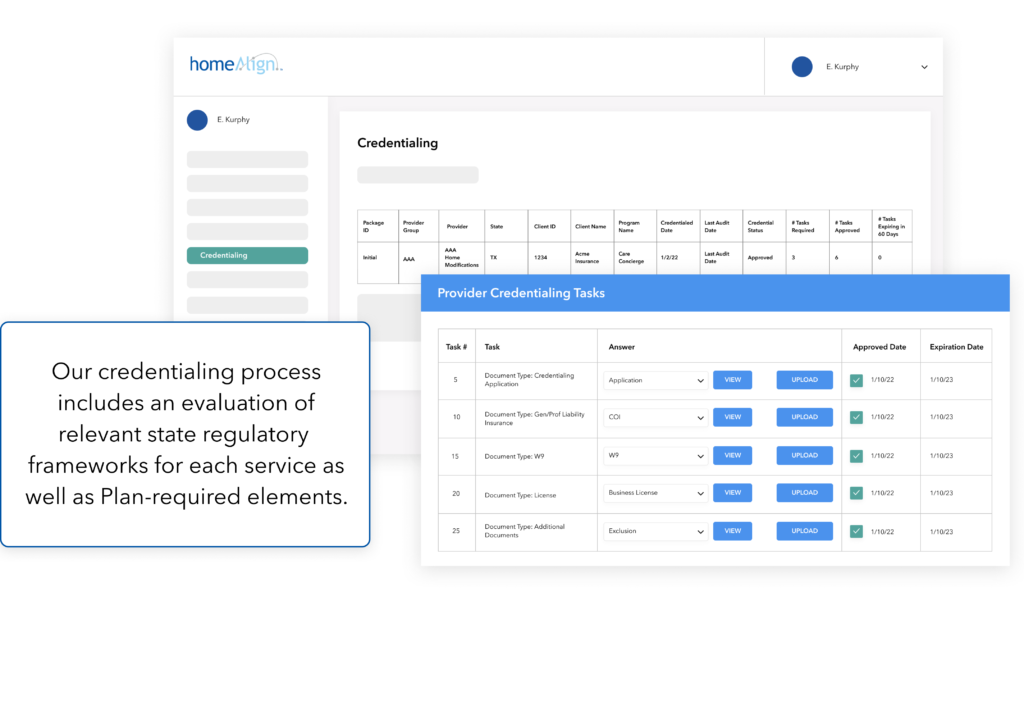
Delivering only the highest quality care and support.
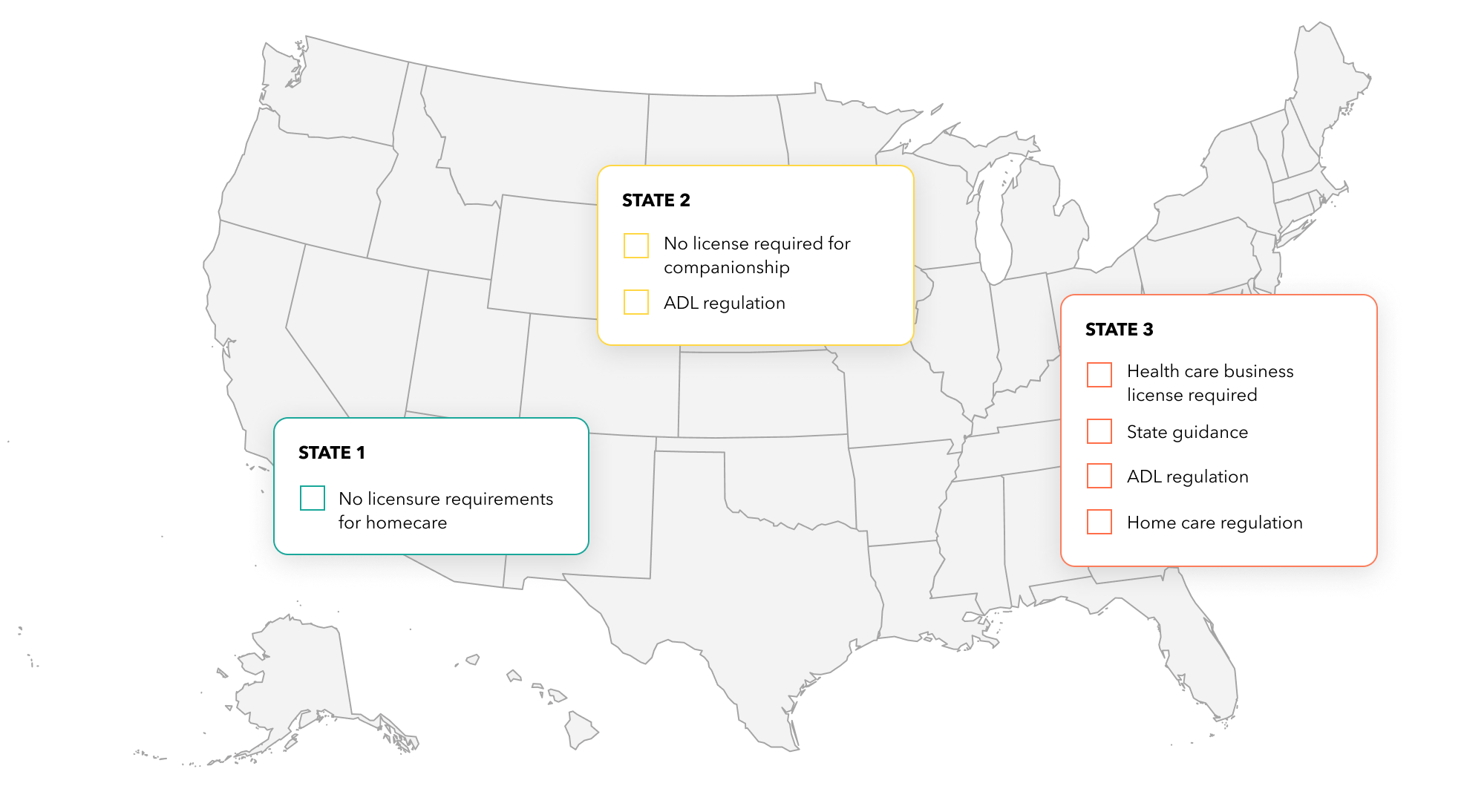
Each care and support service provider is required to undergo our credentialing process. We typically are delegated by our partners to credential our providers, and thus can use either their protocols or a custom-developed process. Our software platform allows providers to self-manage their applications, while our analytics dashboard alerts our team about incomplete applications. Because every state is different, we have built all of our protocols to maintain compliance across all state licenses and regulations.
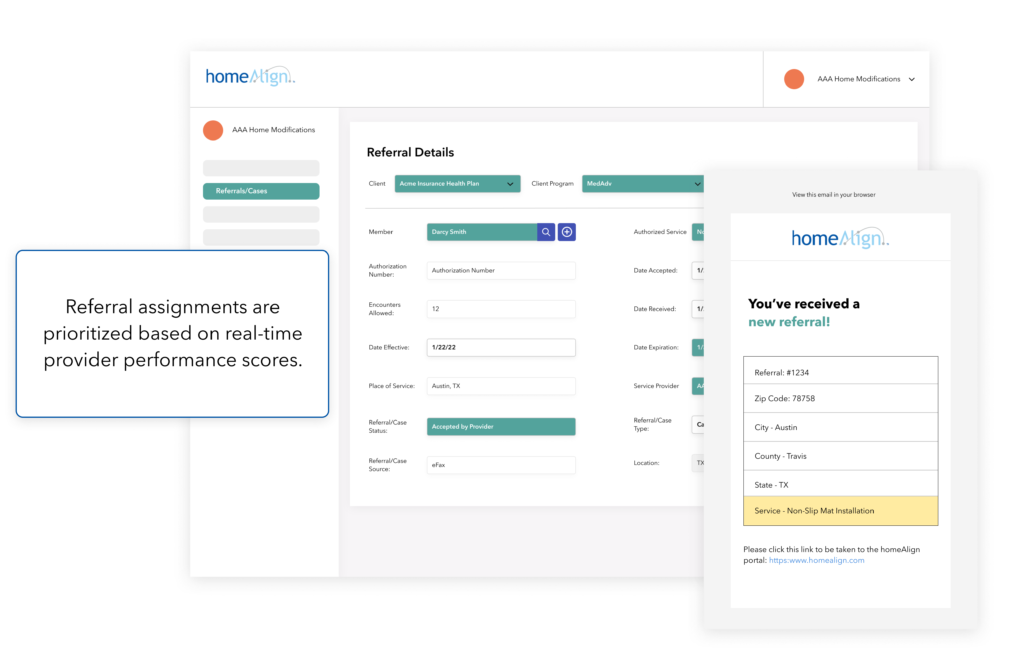
Automated fulfillment and active provider monitoring.
Provider performance scores are determined based on factors like member satisfaction, referral acceptance, fulfillment rates, and timeliness. All future referrals are prioritized and assigned to only the highest-performing providers.
After assignment, our system also monitors fulfillment and triggers escalation alerts if fulfillment does not occur as planned.
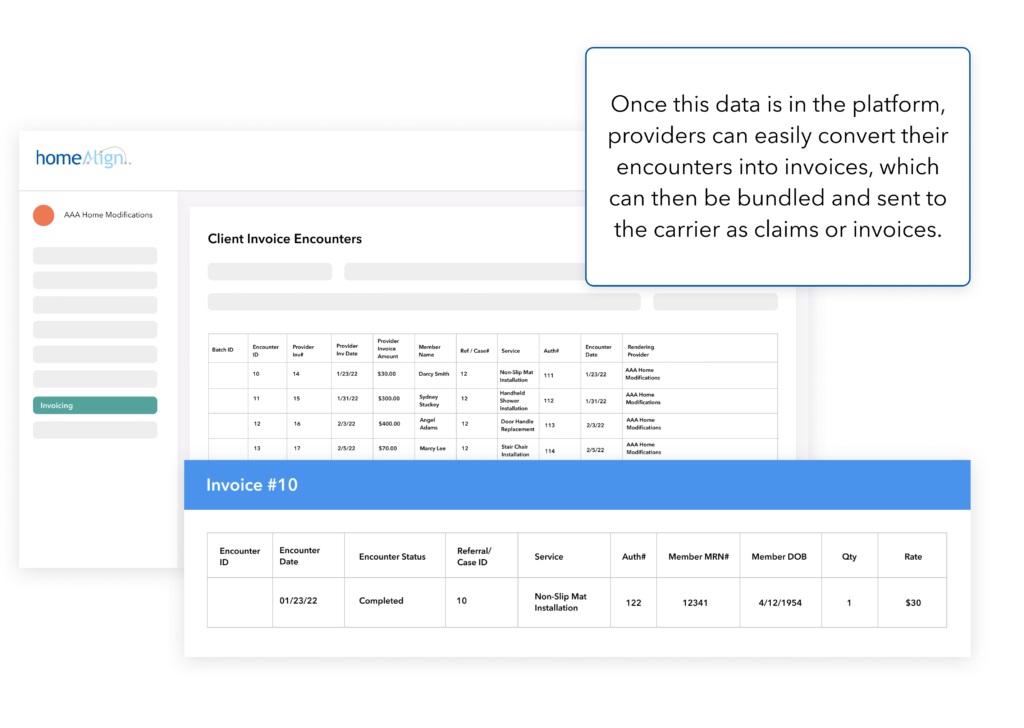
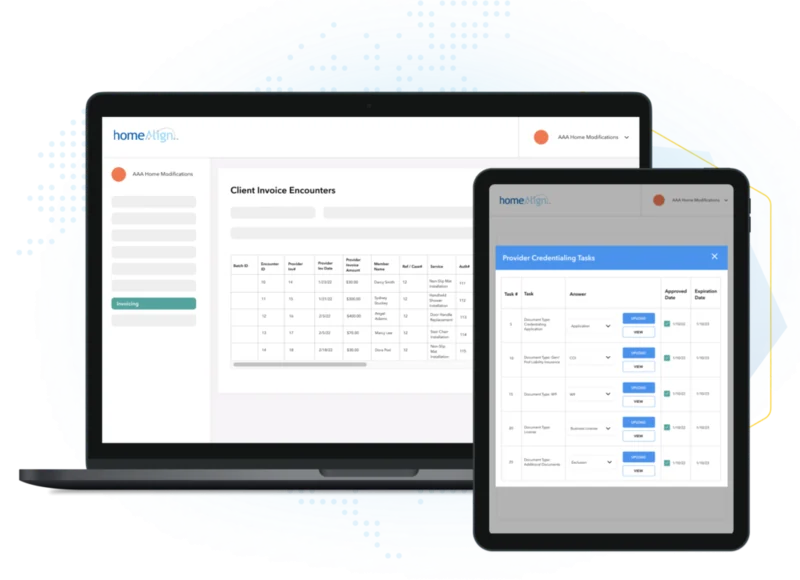
Standardized data and simplified invoicing.
As a condition for payment, providers must submit visit data and documentation through one of the four platform input options. This allows us to organize and standardize the encounter data from many different provider systems.
The regulatory environment for in-home care is complex and ever-changing. We understand the rules and adapt our fulfillment models to ensure compliance with all regulatory bodies.
Contact us to get started.
healthAlign helps you focus on what matters most – better member health outcomes, lower costs, and superior experiences.